Motion Mitigation Strategies in Particle Therapy
When treating tumors in the chest or abdomen with particle therapy, clinicians face a significant challenge: the tumor moves as the patient breathes. Particle beams are extremely precise, delivering most of their energy at a specific depth inside the body. This precision becomes an hurdle when the target moves, as the high-dose region can miss the tumor entirely or hit healthy tissues instead. For some patients, these motion effects can be quite large; tumors can move up to 3 centimeters with each breath, and the shifting tissues cause the beam to stop at the wrong depth. This complex interaction between the moving tumor and the scanned particle beam is known as the interplay effect
The simplest solutions involve trying to reduce or account for motion. Clinicians can use compression belts to limit breathing motion or ask patients to hold their breath during treatment . Another option is to add safety margins around the tumor, planning to irradiate a slightly larger area so that the tumor remains inside the high-dose region even if it shifts. However, this approach partly reduces the precision advantage of particle therapy.
A more sophisticated approach, known as robust optimization, has been developed and is also an active area of our work. Instead of simply adding margins, this technique creates treatment plans that are less sensitive to likely motion scenarios. The planning system tests many possible breathing patterns and uncertainties and finds a solution that maintains good coverage across the most probable situations. Recent work has also investigated combining motion mitigation strategies with online adaptive therapy, enabling daily plan adjustments based on patient-specific motion patterns during treatment .
More advanced techniques actively respond to tumor motion during treatment. Respiratory gating allows the beam to turn on only when the tumor is in the right position, typically when the patient has exhaled and movement is minimal: This approach works well, but makes treatments longer since the beam is off most of the time.
Rescanning delivers the treatment in multiple passes, so if one pass is affected by motion, the others average out the effect. This statistical approach has proven very effective for managing motion-induced dose variations.
Beam tracking represents the most technically challenging approach; the treatment machine continuously follows the moving tumor in real time, adjusting both the beam direction and energy. While promising, this technology requires significant hardware modifications and is not yet widely available clinically.
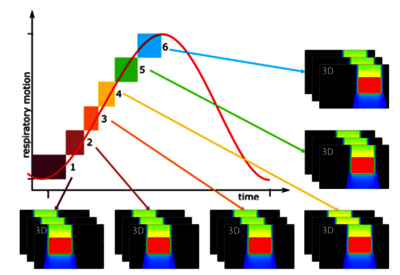
GSI pioneered and first developed the most advanced motion management techniques available today. Multi-Phase 4D (MP4D) ,originally conceived and implemented at GSI, creates separate treatment plans for different breathing phases and delivers them in perfect synchronization with the patient's breathing cycle (Fig. 1).
Building on this foundation, our team further developed MP4DRT, which combines the 4D approach with real-time beam tracking. This hybrid technique allows the delivery of a uniform dose to the target even in the presence of irregular motion. The method has also been tested at CNAO (Centro Nazionale di Adroterapia Oncologica) clinical center in Pavia, Italy, demonstrating its feasibility for patient treatments.
Motion impact and mitigation strategies were also investigated through treatment planning studies to help the transition from the research to the clinic environment. Dosimetric studies, comparing static and motion-degraded plans for multiple patients, allowed us to draw conclusions taking into account inter-patient variability. These studies, both in the context of upright therapy and the lung modulation effect, are current research topics in the Medical Physics group.