Fighting liver and lung cancer with heavy ion therapy
New methods for treating moving tumors
20.03.2024 |
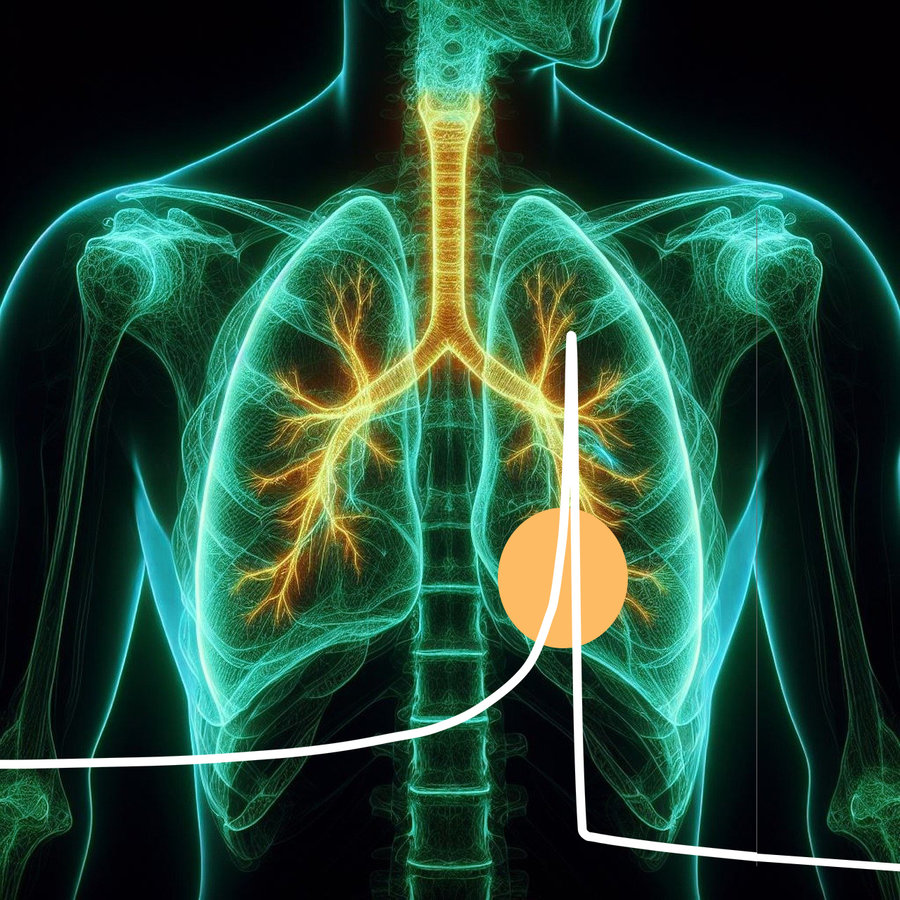
The first patients were treated with heavy ions 25 years ago – whereas therapy was long limited to the head and pelvis, today tumors in the upper body, for example in the lungs, liver and pancreas, can also be treated, even though they are constantly in motion due to breathing. Some methods are already in clinical routine, other developments from the GSI Helmholtzzentrum für Schwerionenforschung offer new hopes and opportunities for cancer treatment.
In order to fully exploit the precision that is possible with heavy ion therapy, patients must be fixed with millimeter precision. However, tumors in the abdomen and chest are constantly in motion due to breathing and the heartbeat. Liver, lung or bowel cancer could therefore not be treated precisely with the heavy ion beam for a long time. However, it is precisely these tumors that could benefit greatly from heavy ion therapy.
Precision in new ways
New methods studied and developed at GSI, such as multiphase optimization and residual tracking, are now on the verge of a breakthrough. These techniques divide the movement of the tumor during breathing into phases in which the position of the tumor is determined. With the help of 4D CT imaging, in which the patient is x-rayed layer by layer, the position and movement of the tumor can be determined for planning the radiation treatment. This allows the radiation to be planned in such a way that it delivers the desired radiation dose to the tumor despite the expected movement. The multiphase optimization developed at GSI achieves a very high dose accuracy for model patients who always breathe in the same way.
The difficulty for clinical application: The respiratory movement assumed during radiation planning never corresponds exactly to the patient's actual breathing during radiation, which sometimes takes place several days after imaging in 4D CT. For example, an accelerated breathing rate or shallower inhalation must be taken into account in order to fully exploit the high precision of heavy ion therapy. The new irradiation technology developed at GSI combines so-called residual tracking with multiphase optimization. This allows the beam to additionally follow the tumor's movements to the right, left, up and down, thus compensating for deviations in tumor movement. Comparative studies have shown that tumors with a combination of these methods are hit very precisely from a clinical point of view. Experiments with plastic phantoms will soon take place at the Centro Nazionale di Adroterapia Oncologica (CNAO) in Italy. The method has already been integrated into the radiation system there and will then be used for patients for the first time.
FLASH treatment
FLASH irradiation, which is also being researched at GSI by the groups led by Ulrich Weber and Walter Tinganelli in the Biophysics Department, is another promising development in which the radiation dose is delivered to the tumor in an extremely short time. This enables the treatment of various types of cancer, as tumors virtually do not move during the 100 milliseconds of irradiation. However, this method requires state-of-the-art imaging technology to ensure that the tumor is hit precisely during the flash irradiation. This technique is being tested in an ongoing study at GSI and MIT in Marburg. Further cooperation with industry partner Varian and the Technische Hochschule Mittelhessen is paving the way for clinical application.
Pragmatic solutions already in clinical use
While clinical trials with the new methods are underway, some pragmatic solutions are already benefiting patients. Several methods that circumvent the problem are now in routine clinical use. One proven method for treating tumors in motion is "gating". The radiation is synchronized to the correct time in the breathing movement and irradiated in the seconds when the patient pauses between exhaling and inhaling. The patient's breathing phase can be recognized either by measuring the respiratory flow through a tube, by a belt that measures the pressure of the upper body during inhalation, or by camera tracking of markings on the patient's body. Another method is to suppress the patient's breathing to minimize the movement of the tumor. Patients can hold their breath and be supplied with oxygen if necessary. In some cases, the patient's lungs are also flooded with oxygen-enriched air, which replaces breathing and can therefore eliminate movement.
These methods are already being used at the Heidelberg and Marburg Ion Beam Therapy Center to treat pancreatic cancer, liver cancer, recurrent rectal cancer, lung cancer and lymphomas, for example.
Imaging is the key
Imaging, i.e. the visibility of the tumor during radiotherapy, is a key factor in achieving a good result. Innovation in image-guided particle therapy is a hallmark at GSI. The Biophysics Department has got two ERC grants on this topic. The Advanced grant BARB to Marco Durante started in 2021 to investigate the use of radioactive ion beams for simultaneous treatment and beam visualization by PET. Professor Christian Graeff was awarded a Consolidator grant in 2023 to open up new treatment options for pancreatic and lung cancer. For the first time, mixed ion beams will enable simultaneous treatment and image guidance. Carbon ions deliver the dose to the target, while helium ions, accelerated simultaneously to the same speed, traverse the patient and indicate the location of the tumor and the radiation distance.
These developments promise major steps forward in radiotherapy for cancer and offer new hope for patients with tumors in the upper body. (LW)